The first wave COVID-19 effort from Government, health, charities, businesses and our population has been extra-ordinary. But with over 8500 deaths, we need to take stock and see if there are ways we can improve for the likely second wave.
It has now become clear that the early days of Canada’s pandemic response were characterized by warnings that were ignored, confusion in the chain of command and delays in building scalable COVID-19 testing, placing orders for PPE and, crucially, the timing and extent of lockdowns.
However, communication problems are common in crises and Canada’s response may have been no worse than others.
One way of quantifying the possible impact of these difficulties and identifying areas for improvement is to compare outcomes in Canada such as COVID-19 death rates to other high-income countries where, like us, the first wave is coming to an end.
COVID-19 death rates vary considerably.
According to data posted by John’s Hopkins on June 25, Canada’s rate was 23 deaths per 100,000 population which outperforms many including UK, Italy, Spain and Sweden that had death rates 2-3 times higher than ours. We also out-performed France, Netherlands, Ireland and, of course, the USA. But a number of countries had lower death rates and Germany’s death rate was half of ours.
Being in the middle of the pack may seem OK. But from this doctor’s perspective it is not good enough. And the need to improve is made clearer by a new sort of calculation – a comparative lives lost analysis which shows that we would have saved 4528 Canadian lives if we had the same COVID-19 death rate as Germany.
Comparing countries can be difficult. For instance, the COVID-19 death rate in Germany could be lower because they tested fewer people and under-diagnosed COVID-19. It could be linked to demographic differences; if Germany had fewer elderly people the rate would be lower because they are the highest risk group for COVID-19 death. It could also be because of the timing of their pandemic; if Germany had its first COVID-19 case later than Canada, it may have had better information and more time to mobilize.
None of these stand up. Germany has a similar COVID-19 testing rate to Canada; it has a 30 per cent larger elderly population; and, the first cases in both countries were on January 27, 2020.
It is more likely that the differences in deaths are because of our pandemic response. Particularly, how we supported long-term care (LTC) homes and the timing and extent of our lockdowns.
Eighty-one per cent of Canada’s COVID-19 deaths have been in LTC homes compared to 34 per cent in Germany.
The poor quality of some of our LTC homes and the lack of proper inspection in some Provinces is a national disgrace. Last week’s report from the Canadian Institute for Health Information concludes that the countries that did the best jobs in protecting older people in LTC were those with centralized regulation and organization of LTC and those that implemented strict LTC guidelines on COVID-19 prevention at the same time as their lockdowns.
Delay in implementing lockdowns leads to an increased severity of pandemic. Germany has a national pandemic plan developed by the Robert Koch Institute which gives the states clear guidance on what they should do when. This led to earlier and more comprehensive lockdowns than in Ontario and Quebec.
If we had better supported LTC and if there had been no delay in lockdowns, Canada would be much closer to Germany’s COVID deaths rate. We would have saved thousands of lives.
If we want to be as effective as Germany in protecting our population in the second wave, we need to ensure that decisions such as lockdowns are made quickly and effectively. We need urgently to improve LTC, but, the broader lesson to learn is that we need to have stringent guidelines, testing, tracing and isolating in place for emergent at-risk groups – it was older people last time but will likely be those in other congregate living settings and racialized populations in the next wave.
COVID-19 so far has not been as bad as it could have been, but our response has not been as good as it should have been. Doing the different sort of analysis that we have done here – a comparative, lives lost analysis – puts Canada’s response into sharp relief. It moves us away from reporting what feels like a sanitized reporting of illness rates towards shining a light on the real toll of this crisis and the impacts of the political and public health decisions that have been made.
There are 4528 lives lost that may have been saved. We can and should do better.
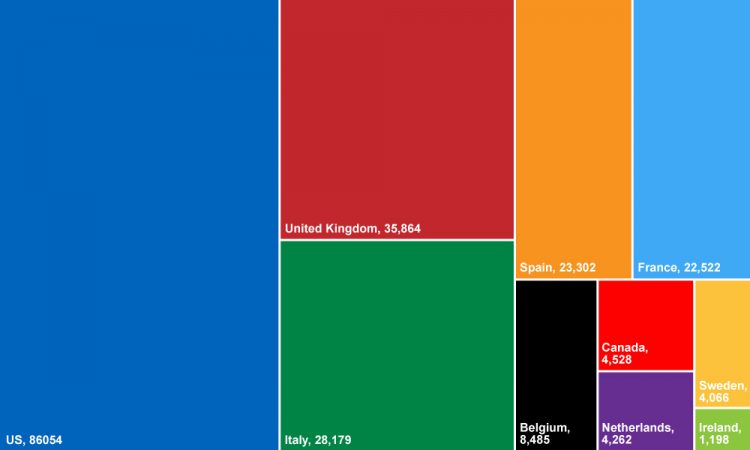
Number of lives that could have been saved if each country’s response was the same as Germany. Calculated from John’s Hopkins data, June 25.
We are grateful to Dr. Natasha Crowcroft for the June 25, 2020 analyses used in this blog.
