Over the past few weeks, we have looked at where the federal parties stand on several key issues that affect Canadians’ health: PharmaCare, housing, jobs and income and early childhood education and care. In this final health equity impact assessment of our series we look at issues that the parties aren’t talking about and that deserve more attention.
Health equity impact assessments support decision makers to incorporate health and health equity in all policies by identifying potential health impacts and enhancing positive impacts while reducing negative impacts. Using a health equity impact assessment tool 1 we identified populations that may experience differential health risks of particular policies, such as people with low income, racialized Canadians and people with disabilities. We then identified specific determinants of health and health inequities that should be considered. Based on this analysis, this election-focused health equity impact assessment identified four areas that the parties should be discussing to improve health equity in Canada: income inequality, health care, good data and population health and social inclusion. We also call for all parties to set out a vision of a healthy Canada for all.
Income Inequality
Conversation in this election has focused squarely on what each party would do for Canada’s middle class, from tax policy to child care policy to infrastructure policy. Lost among this rhetoric, however, has been discussion of increasing income inequality in Canada and what that means to our society and our health.
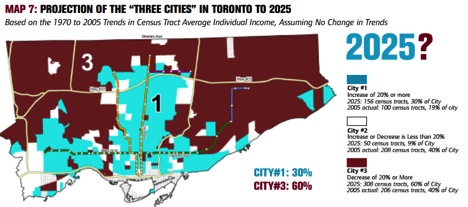
Source: J. David Hulchanski, The Three Cities Within Toronto: Income Polarization Among Toronto’s Neighbourhoods, 1970-2005, Cities Centre, University of Toronto.
Income inequality can have serious health impacts. A Canadian study found that women living in highly unequal urban centres were 26 percent more likely to die of lung cancer and more than two times more likely to die of transport injuries or alcohol-related causes than women living in more equal urban centres. Men who lived in unequal cities were 50 percent more likely to die of alcohol-related causes and 20 percent more likely to die of colorectal cancer.2 Income inequality has also been connected with increased risk of anxiety depression, and suicide. 3
Canada is becoming an increasingly unequal society. In Toronto, wealth has been concentrating in the central city and along subway lines in recent decades, with poorer Torontonians living in the Northeastern and Northwestern corners of the city and middle income neighbourhoods rapidly disappearing altogether, leading to income polarization.4 Similar income polarization patterns are found in Vancouver 5 and in Montreal. 6 These trends suggest that health impacts of income inequality will worsen in coming decades.
The federal government can play a major role in reducing income inequality through tax increases for high earners and mechanisms like Old Age Security, Guaranteed Income Supplement, Canada Pension Plan and the Working Income Tax Benefit. But for people living with low income access to services may also be an important tool. The government can reduce inequality and improve health by improving the provision of services, including housing, child care, transportation and education. The parties have been talking about many of these things and how they can benefit the middle class. But to improve the health of Canadians it would be better if platform commitments considered what would benefit our society as a whole.
Health Care
Surprisingly little attention has been paid to how to improve health care systems across Canada. Our system was recently ranked 10th out of 11 in a study of OECD countries, outperforming only the United States. Timeliness of care and system efficiency were particular issues.7 Our per capita spending on health care is high so we should be able to improve performance.8
Access to high quality health care services is important to overall health. While the Canada Health Act sets out the basic requirements that provincial governments must meet – public administration, comprehensiveness, universality, portability and accessibility – access to health care services varies across Canada and across socio-demographic lines. The bottom third of income earners in Canada are half as likely to see a specialist when required than the top third of income earners, 50 percent more likely to face difficulties receiving care in the evening or weekends and 40 percent more likely to wait five or more days for an appointment with a doctor.9
The federal parties have made important, but limited, commitments to improving Canada’s health care system. The NDP has proposed establishing national prescription drug coverage and would invest in improving youth mental health services. The Liberal Party has committed to creating a new health accord between the federal and provincial government, invest $3 billion over four years to improving home care services, supporting provinces to bulk purchase prescription drugs, and introducing a National Disabilities Act. The Green Party would reengage the provinces for a new health accord, expand prescription drug coverage to cover all Canadians, establish public dental coverage for low income children and work with provinces to develop preventative health care guidelines. The Conservative Party has not made any health care commitments.
Each of these commitments has merits, but missing from the discussion is a clear articulation of what we expect from our health care system or a vision of what Canada’s health care system could become. A recent report prepared for the government by the Advisory Panel on Healthcare Innovation set out the challenges facing Canada’s health care system and made recommendations on how to turn our system around, including by testing new forms of payment where care is organized and financed around the needs of patients, integrating delivery arrangements to address social needs and social determinants of health and joining the pan-Canadian Pharmaceutical Alliance.10 None of the parties have addressed this critical document or set out their own vision for a high-performing health care system.
Reforming health care systems to increase access to care is important, but real population health gains can only be realized by bending the cost curve and moving our focus upstream to the broader determinants of health. Incorporating a Health in All Policies approach to policy decisions is a key mechanism to make this shift in perspective. We need to address the inequities in risk factors for illnesses and illness prevention and health promotion has been demonstrated to be effective in making this shift. 11 The federal government should increase the role of the Public Health Agency of Canada, Health Canada and the Mental Health Commission of Canada. This would place the federal government as leaders in illness prevention and health promotion and would support provinces to move upstream.
Population health and good data
Canada has an incredibly diverse population which greatly enriches our social fabric, but not everyone in Canada has the same access to good health. Canadians who fare poorly in the social determinants of health face health risks not shared by other Canadians. Aboriginal status, gender, race and disability are all important determinants of health and other populations like recent immigrants face disproportionate burdens on their health.12 Belonging to a health disadvantaged population can compound health inequities connected to other determinants of health like living in poverty and experiencing food insecurity.
What’s measured matters, but in this election little attention has been paid to the need to improve the quality of disaggregated data that can help to understand and address the causes of poor health experienced by many Canadians. The Liberal Party, Green Party and NDP have all committed to reinstate the mandatory long-form census which would improve data quality in Canada. Beyond this, there is more that the federal government can do to improve data quality. We need better information about how our health care system performs at the population level and whether our social safety net meets the needs of diverse populations. Improving health and health equity for all Canadians requires federal leadership to collect and disseminate good data in addition to making federal transfers conditional on provinces collecting, reporting and acting on health equity data.
Social inclusion
Feeling included and valued in society is an important determinant of health. Experiencing social exclusion can have direct negative health impacts that manifest in increased stress and anxiety. Stress has been shown to impact a range of health outcomes, from increased susceptibility to the common cold to increased mortality rates.13 Social exclusion can also create barriers to other critical determinants of health like employment, adequate income, education and housing. Some populations are at greater risk of experiencing social exclusion, including recent immigrants, LGTBQ populations and racialized Canadians.14
None of the federal parties have addressed social inclusion in Canada. The federal government has a particularly important role to play in ensuring that new Canadians feel included and valued in their new home. This could mean increasing the number of refugees eligible for resettlement support and ensuring access to employment supports, adequate housing, health care services and high quality language instruction.
Vision of a healthy Canada
There is scarcely an aspect of federal policy that does not impact health and well-being for Canadians, from health and social transfers to trade to infrastructure priorities. While the four main parties have made commitments in a number of these and other areas, no parties have yet clearly set out what a healthy Canada looks like and how they would go about improving the health of all Canadians.
The federal government has a role to play in reducing health inequities. Too often Canadians consider health to be a provincial responsibility, but this confuses health and health care. All governments – federal, provincial and municipal – have a role to play in addressing health equity and the social determinants of health in Canada. The federal government should lead by example and should foster strong partnerships with other levels of government to improve the health of all Canadians.
Download: What the Parties Arent talking AboutWhat the Parties Arent talking About
- ONTARIO MINISTRY OF HEALTH AND LONG-TERM CARE 2012. Health Equity Impact Assessment. Toronto. ↩
- AUGER, N., HAMEL, D., MARTINEZ, J. & ROSS, N. A. 2012. Mitigating effect of immigration on the relation between income inequality and mortality: a prospective study of 2 million Canadians. J Epidemiol Community Health, 66, e5. ↩
- MANSEAU, M. W. 2014. Economic Inequality and Poverty as Social Determinants of Mental Health. Psychiatric Annals, 44 ↩
- HULCHANSKI, J. D. 2010. The Three Cities Within Toronto: Income Polarization Among Toronto’s Neighbourhoods, 1970-2005. Cities Centre, University of Toronto ↩
- LEY, D. F. & LYNCH, N. A. 2012. Divisions and Disparities in Lotus-Land: Socio-Spatial Income Polarization in Greater Vancouver, 1970-2005. Cities Centre, University of Toronto. ↩
- ROSE, D. & TWIGGIE-MOLECEY, A. 2013. A City-Region Growing Apart? Taking Stock of Income Disparity in Greater Montréal, 1970-2005. Cities Centre, University of Toronto ↩
- THE COMMONWEALTH FUND 2014. US Health System Ranks Last Among Eleven Countries on Measures of Access, Equity, Quality, Efficiency, and Healthy Lives. New York, NY: The Commonwealth Fund. ↩
- ORGANIZATION FOR ECONOMIC COOPERATION AND DEVELOPMENT 2015. Country Note: How does health spending in Canada compare? : Organization for Economic Cooperation and Development. ↩
- MIKKONEN, J. & RAPHAEL, D. 2010. Social Determinants of Health: The Canadian Facts. Toronto: York University School of Health Policy and Management ↩
- ADVISORY PANEL ON HEALTHCARE INNOVATION 2015. Unleashing Innovation: Excellent Healthcare for Canada. Ottawa: Health Canada ↩
- WEARE, K. & NIND, M. 2011. Mental health promotion and problem prevention in schools: what does the evidence say? Health Promotion International, 26, i29-i69.;FUNG, C., KUHLE, S., LU, C., PURCELL, M., SCHWARTZ, M., STOREY, K. & VEUGELERS, P. 2012. From “best practice” to “next practice”: the effectiveness of school-based health promotion in improving healthy eating and physical activity and preventing childhood obesity. International Journal of Behavioral Nutrition and Physical Activity, 9, 27.; HEATH, G. W., PARRA, D. C., SARMIENTO, O. L., ANDERSEN, L. B., OWEN, N., GOENKA, S., MONTES, F. & BROWNSON, R. C. Evidence-based intervention in physical activity: lessons from around the world. The Lancet, 380, 272-281 ↩
- MIKKONEN, J. & RAPHAEL, D. 2010. Social Determinants of Health: The Canadian Facts. Toronto: York University School of Health Policy and Management ↩
- COHEN, S., DOYLE, W. J., SKONER, D. P., RABIN, B. S. & GWALTNEY, J. M., JR. 1997. Social ties and susceptibility to the common cold. Jama, 277, 1940-4.; ROSENGREN, A., ORTH-GOMÉR, K., WEDEL, H. & WILHELMSEN, L. 1993. Stressful life events, social support, and mortality in men born in 1933. BMJ : British Medical Journal, 307, 1102-1105. ↩
- STANDING SENATE COMMITTEE ON SOCIAL AFFAIRS, SCIENCE AND TECHNOLOGY 2013. In From the Margins, Part II: Reducing Barriers to Social Inclusion and Social Cohesion ↩